What Is PCOS? The Reproductive Disorder That Doctors (Wrongly) Try To Treat With The Pill
I can remember exactly where I was, what I was doing, what I was looking at when my doctor called and told me that I had PCOS (polycystic ovarian syndrome). I was shocked.

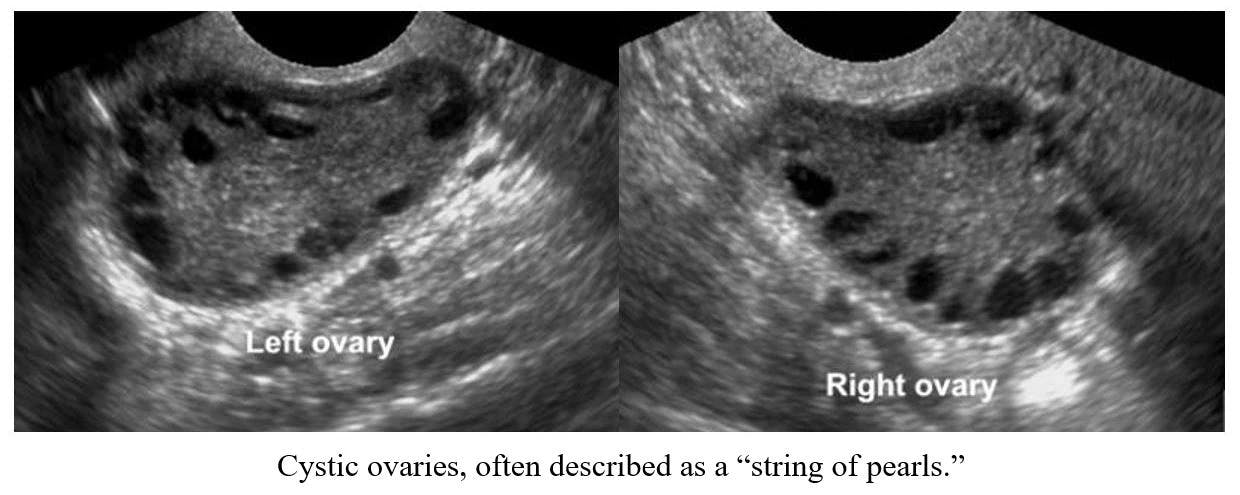
I had never considered PCOS (even though I knew something was wrong with me because I’d been trying unsuccessfully to get pregnant for years) because I didn’t exhibit any of the major symptoms. But my doctor had proof in my ultrasound images — my ovaries were full of cysts.
The most common cause of female infertility, Polycystic Ovarian Syndrome (PCOS) is generally considered a hormonal disorder that affects the ovaries. However, others like Dr. Jolene Brighten and Dr. Andrea Dunaif say it’s more of a metabolic disorder that has hormonal side effects. This ambiguity is characteristic of the condition. There are still so many unknowns — from the cause to the cure — that it can be frustrating for the many women diagnosed with it.
What Is PCOS?
Basically, PCOS is an anovulatory condition — meaning that a woman doesn’t ovulate at all or ovulates irregularly. In a healthy cycle, after your period, follicle stimulating hormone, luteinizing hormone, and estrogen trigger the development and the release of an egg from a follicle in your ovary. The follicle then forms what’s called the corpus luteum and produces progesterone. When the level of progesterone falls, you get your period, and the cycle begins again.
But in women with PCOS, the egg doesn’t get released from the ovary and instead becomes a cyst (a fluid-filled sac). This cyst then produces androgens (a group of hormones present in high levels in men, including testosterone), at a much higher level than is normally found in a woman. The abnormally high level of androgens causes the other symptoms of PCOS and, together with the lack of progesterone, perpetuates the woman’s out of whack menstrual cycles.
Who Can Have It?
According to the Office of Women’s Health, 5-10% of women of childbearing years (ages 15-44) have PCOS. Women of all races can have it. PCOS also seems to be genetically transmittable somehow, so if your aunt, mother, or sister has PCOS, you’re much more likely to have it too.
The Signs of PCOS and Getting Diagnosed
PCOS has many symptoms, which contributes to the difficulty of getting diagnosed. Not every woman with PCOS will exhibit all or the same symptoms, and the symptoms range in severity. In fact, one survey showed that almost 50% of PCOS patients saw at least three doctors before getting a diagnosis, and 33% of them said it took more than two years. Personally, it took me two doctors and four years to get a diagnosis.
Symptoms:
Acne and/or oily skin
Male hair patterns (balding or facial hair/body hair)
Thinning hair on head
Irregular cycles/irregular bleeding
Obesity and/or difficulty losing weight
Insulin resistance
Chronic inflammation
Elevated estrogen levels
Excess androgen hormones
Low thyroid hormones
Cysts in ovaries
Infertility
Out of this long list, most doctors use just three symptoms to diagnose. These are called the Rotterdam criteria, in which doctors look for elevated androgen levels, irregular/absent cycles, and cysts in the ovaries. If two of these three symptoms are present, the woman is diagnosed with PCOS.
However, doctors who specialize in PCOS (like Dr. Lara Briden and Dr. Fiona McCulloch) acknowledge that there are up to five distinct expressions of PCOS, in which different combinations of symptoms present different “phenotypes” of PCOS, each requiring different tests and treatments.
Out of the long list of symptoms, most doctors use just three to diagnose.
For example, one basic difference is an insulin-resistant PCOS case versus a non-insulin-resistant one. Insulin resistance is when your muscle, fat, and liver cells don’t respond effectively to insulin and can’t take the glucose from your blood to be used as fuel or to be stored (resulting in high blood sugar). The insulin-resistant PCOS woman will struggle with obesity and weight loss, and will have a much higher risk of developing type II diabetes. A key part of her treatment will be insulin regulation and weight loss. But a woman who has non-insulin-resistant PCOS doesn’t need this treatment. The components of her PCOS might be excess androgens, thyroid problems, and inflammation, which will need to be addressed differently.
What Causes PCOS?
Officially, the cause of PCOS is “unknown.” But several scientific theories have surfaced from research:
An excess of anti-Müllerian hormone present in mothers with PCOS during pregnancy seems to trigger PCOS in the female offspring. This seems to explain why PCOS runs in families.
The stimulation of androgen receptors in the brain seems to play a key role in the onset of PCOS.
Chronic stress during childhood development can cause PCOS because the stress hormone pathway directly interferes with the reproductive hormone pathway.
Evolutionarily-developed, advantageous, biological features (like insulin resistance, which would have helped in times of starvation) that are genetically passed down are also considered a cause of PCOS.
PCOS Is Incurable, but Not Hopeless
Because there is no known, single cause for PCOS, there is no single cure or even treatment. Women who are diagnosed with PCOS are diagnosed with a lifelong condition, and each woman’s case will need treatment tailored to her unique combination of symptoms. The good news is that almost all treatments are easily accessible.
The top recommendation from the American College of OB/GYNs for living with PCOS is lifestyle changes. This includes regular exercise (which manages stress and lowers cortisol and adrenal levels, regulates sex hormones, and aids in weight loss and regaining insulin sensitivity) and diet changes to reduce inflammation (no gluten, and little to no dairy and sugar).
The top recommendation for living with PCOS is lifestyle changes, which includes regular exercise and an anti-inflammatory diet.
Some medications or supplements might be recommended or prescribed. Metformin or myo-inositol are commonly prescribed for insulin resistance. Supporting low hormones with bioidentical hormone supplementation at the appropriate times of the cycle helps restore a healthy menstrual cycle (for example, taking bioidentical progesterone after ovulation). Many women with PCOS also have thyroid issues and will need medication (I’m on two different thyroid meds). Some women love using essential oils to promote relaxation and support healthy hormone function naturally.
Surgery is another option, depending on your health goals, but not all surgical procedures are the same. I personally have had great success with my ovarian wedge resection surgery done by a NaProTechnology trained surgeon. (I love this methodology because it views irregular cycles and infertility as symptoms of an underlying cause and focuses on treating that root problem, not just prescribing the Pill to manage symptoms.) I’m still cyst free four years post surgery! This surgery has a more than 80% success rate in getting pregnant post procedure, if that’s your goal. If you just want to reset your cycles, it can do that too. Another benefit of this surgery is that the doctor can check for endometriosis at the same time, because half of women with PCOS also have endometriosis (I did).
PCOS and the Pill
So what about hormonal birth control? It’s commonly prescribed to treat acne and irregular cycles. But for women with PCOS, it’s not a helpful solution at all.
A birth control pill pack has estrogen and progestin (which is NOT progesterone). Progestins are chemically more similar in structure to testosterone than progesterone. Remember that women with PCOS tend to have high estrogen levels already (so they don’t need more estrogen put into their bodies), and they have elevated levels of testosterone/androgens (so, again, they don’t need more testosterone-like hormones, e.g. progestins, put into their bodies). Progestins link with androgen receptors and can cause excess androgen side effects, which is already a problem with PCOS. So the hormonal ingredients of the Pill can actually make PCOS worse by exacerbating the hormonal imbalance and the symptoms.
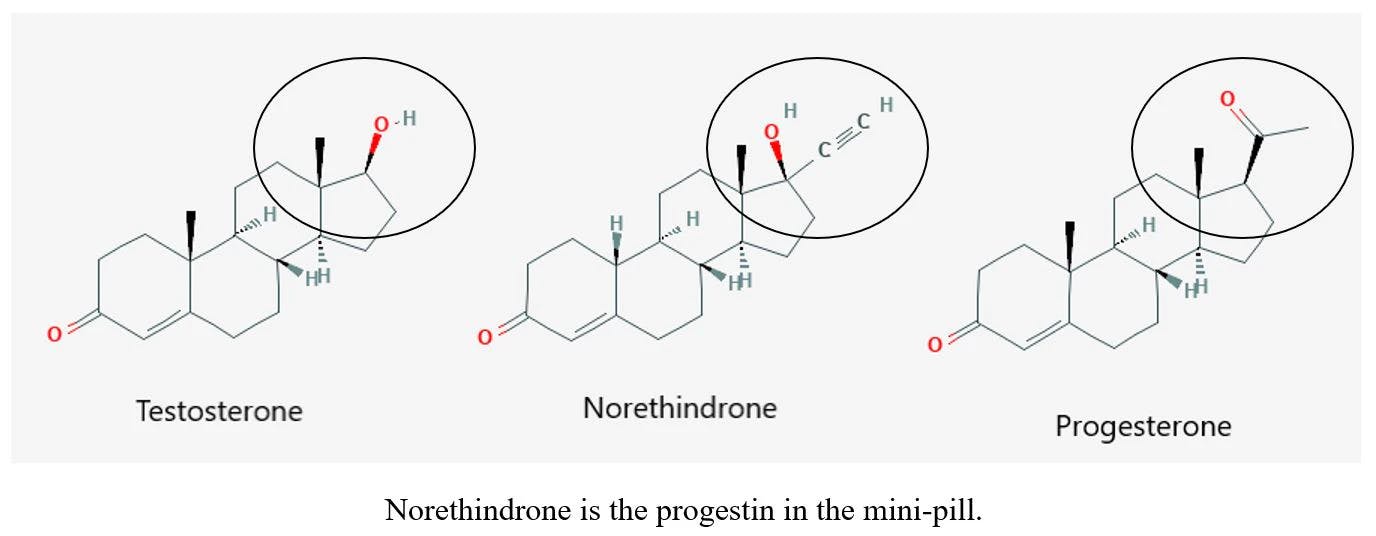
What women with PCOS do need is bioidentical progesterone, because their ovaries aren’t producing enough because they aren’t ovulating and forming the corpus luteum (which in turn messes up her cycle). So to regulate her cycle, a woman with PCOS would be better served by taking a bioidentical progesterone supplement post ovulation (which comes from Mexican yams, who knew?). It’s way more natural and healthy and works with her body. Plus, adding more progesterone to the body post ovulation is a natural and healthy way to get rid of PMS (It made mine disappear!).
The hormonal ingredients of the Pill can actually make PCOS worse by exacerbating the hormonal imbalance and the symptoms.
Additionally, according to Dr. Jolene Brighten, the Pill causes an array of harmful side effects that all exacerbate PCOS: it affects your thyroid and your adrenals, it’s inflammatory, it affects your mood, it depletes nutrients from your body, it interferes with your brain communicating with your ovaries, it impacts your liver’s ability to regular blood sugar, and it increases your risk of stroke, heart attack, and diabetes (which women with PCOS are already at risk for).
Finding Answers for PCOS in the Future
Hopefully, more money will be dedicated to researching PCOS in the future. (Currently PCOS research receives less funding than rheumatoid arthritis, tuberculosis, and lupus, three other disorders with similar or lower rates of prevalence and death.) Increasing awareness in the medical community and the culture at large would help, and celebrities like Daisy Ridley, Victoria Beckham, and Emma Thompson who have been open about their struggles with PCOS are doing just this.
However, modern feminism isn’t helping by removing the focus from motherhood. The more lobbying and advocacy there is for a cause, the more research money it gets from the government and the NIH. And feminists are focusing their efforts on abortion and contraceptives, not the actually reproductive parts of their reproductive rights. Even mainstream modern feminists who struggle to get pregnant feel ignored by their own cause.
Closing Thoughts
It’s important to remember that getting a PCOS diagnosis is not getting a sentence of doom. It’s still completely possible to have a healthy, fulfilling life. It’s still highly possible to get pregnant. You might have to do more research on your own, make some lifestyle changes, and be your own advocate in the doctor’s office or find a more educated doctor. But being more informed about your body will help you feel more in control. With modern technology and medicine, we have the best shot in history to achieve our personal goals of having good health and children.